AMOR-IPAT
Background
AMOR-IPAT [1] is a method of care that aims to safely lower cesarean delivery rates (and lower rates of other adverse birth outcomes) through the regular use of risk-based preventive labor induction. Simply put, AMOR-IPAT uses a risk scoring system to estimate, for each pregnancy, an upper limit of the optimal time of delivery (UL-OTD [2]). The UL-OTD is never greater than 41 weeks 0 days of gestation and is rarely lower than 38 weeks 0 days of gestation. AMOR-IPAT increases the chances that women deliver on or before their individual UL-OTD by offering them preventive induction of labor (pIOL [3]) if spontaneous labor does not develop by 2-3 days before the UL-OTD.
The potential value of AMOR-IPAT is reflected in the results of 5 published retrospective studies and 1 published randomized clinical trial (see below). In these studies, rates of both cesarean delivery and NICU admission, and rates of several other important adverse birth outcomes, were significantly lower following exposure to AMOR-IPAT. Additional studies of AMOR-IPAT are ongoing, and the results of these studies appear to be consistent with the findings of the six published studies.
The relative safety of preventive labor induction in the 38th week of pregnancy has been presented nationally and internationally in abstract form. A full-length manuscript dealing with the relative safety of preventive labor induction in the 38th week of gestation is currently under construction. A poster presenting the data to be used in this study is available here.
Theory
It is well known that rates of adverse birth outcomes (C/S, NICU admission, meconium passage prior to birth, meconium aspiration syndrome, and intra-uterine fetal demise [IUFD]) increase as a function of increasing gestational age during the term period of pregnancy. If cesarean delivery can be viewed as a proxy for non-normal parturition, and if one considers a variety of factors that are at play in the utilization of cesarean delivery—especially increasing gestational age—then the idea of using risk-based preventive labor induction (AMOR-IPAT) as a means of improving birth outcomes becomes plausible.
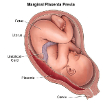
Specifically, the two most common reasons for cesarean delivery are cephalo-pelvic disproportion (CPD – fetus too large for mother’s pelvis, which is the most common reason for failure to progress during labor) and utero-placental insufficiency (UPI – placenta too old to adequately support the fetus during labor, which is the most common reason for fetal intolerance of labor). However, CPD occurs with increasing frequency during the term period. This is because the fetus continues to grow larger as term pregnancy progresses (usual weight gain 5-7 ounces per week). In addition, UPI occurs with increasing frequency during the term period. This is because—starting at around 39 weeks 0 days of gestation—placental function peaks and then begins to deteriorate (slowly at first, and quite rapidly after 41 ½ weeks of gestation). In addition, certain identifiable obstetric risk factors—factors known to be associated with higher risk of cesarean delivery—probably accelerate fetal growth and/or placental aging. With reference to CPD risk, high maternal gestational weight gain, gestational diabetes, and maternal short stature interact with increasing gestational age to create very high risk states for obstructed labor in the late term period of pregnancy. With reference to UPI risk, cigarette use, chronic hypertension and anemia interact with increasing gestational age to create very high risk states for fetal intolerance of labor in the late term period.
CPD and UPI are very different pathways to cesarean delivery, but both CPD and UPI occur at variable rates during the term period as a function of both identifiable risk factors and gestational age. The estimation of a UL-OTD for every pregnancy is an attempt to capture the interaction between a given woman’s personal pregnancy risk profile and the impact of increasing gestational age on birth outcomes that will occur in pregnancies of that type during the term period.
Generally speaking, the greater the quantity and quality of risk factors carried in a given pregnancy, the earlier in the term period it would ideally enter labor. Accordingly, instead of using 41 weeks 0 days for all pregnancies as a time that labor induction should be initiated if a pregnancy is still undelivered (assuming that there has been no reason to perform an “indicated” labor induction), AMOR-IPAT uses the individualized UL-OTD to estimate optimal labor timing. Hence, using AMOR-IPAT, women may be more likely to enter labor when their fetus is more likely to be able to pass through the maternal pelvis and/or when their fetus is more likely to tolerate the considerable stress of labor.
Almost all studies that are used to support the belief that labor induction is by itself harmful and should not be used unless the “benefits” of its use outweigh its “risks” have been retrospective cohort studies. In these studies, the outcomes of women that were induced are compared to the outcomes of women who developed spontaneous labor. However, because most inductions are initiated because there is at least some concern about an increased risk state (all indicated labor inductions, suspected LGA fetus, borderline blood pressure elevations, borderline low amniotic fluid level, mild gestational diabetes), it should be clear that such studies are all potentially confounded by indication. Is it the induction itself that leads to higher rates of adverse birth outcomes, or the reason the induction was initiated in the first place? High quality randomized clinical trials of early-to-midterm non-indicated labor induction have not been performed. However, a 270 subject randomized clinical trial comparing AMOR-IPAT exposure to the current standard of care found statistically significant reductions in the AMOR-IPAT exposed group for both the rate of NICU admission and group Adverse Outcome Index (AOI) score (see attached poster).
Other Key Issues
The use of AMOR-IPAT involves the regular use of early or mid-term risk-based labor induction (38 weeks 0 days of gestation to 39 weeks 6 days of gestation). Two controversial issues other than the relative risk or benefit of non-indicated labor induction need to be addressed.
First, some women identified as being candidates for preventive labor induction will have an unfavorable uterine cervix (Bishop’s score < 6). It has been the experience of the AMOR-IPAT project that while such women are at increased risk for cesarean delivery if they proceed with preventive induction—as compared to the risk of cesarean delivery in the general population—the personal risk for cesarean delivery in such women appears to be reduced if they proceed with preventive labor induction rather than proceed with expectant management. Simply put, for women with both an unfavorable cervix and a personal constellation of risk factors suggesting the potential benefit of a preventive induction, the impact of increasing gestational age may be greater than the impact of having a preventive labor induction in the presence of an unfavorable cervix. Most, but not all, labor inductions complicated by an unfavorable cervix can have that problem adequately addressed through the use of various ripening techniques (PGE1 products, PGE2 products, or mechanical dilators), and considerable medical research has focused on methods available to “conquer” the unfavorable cervix. AMOR-IPAT makes use of that medical research. It is important to realize that the presence of an unfavorable cervix in early term pregnancy is often a problem that is not resolved by the time a post-dates “indicated” induction is needed, and if the attempt at induction is delayed until the late-term period, then problems related to cervical ripening are compounded by the presence of a larger fetus and an older placenta.
Second, AMOR-IPAT often identifies the UL-OTD to be in the 38th week of gestation. Preventive labor induction in the 38th week of gestation is currently not either recommended or allowed in many institutions due to concerns about fetal brain and lung immaturity. However, there is no reason to think that a fetal human brain—which is obviously smaller at 37-38 weeks gestation than it will be at 40 weeks of gestation—will not grow just as fast in the extra-uterine environment as it does in the intra-uterine environment. Furthermore, the research that is used to support the current restrictions on pre-39 week labor induction is sub-optimal.
The first type of sub-optimal research is environmental studies. Environment studies “show” that babies born in the 37th or 38th week encounter higher rates of morbidity (NICU admission, intubation), and the authors of such studies have concluded that therefore non-indicated labor induction—even in the setting of considerable prenatal risk—should be avoided in the 37th and 38th week. However, such studies have failed to consider that there are reasons that promote early term labor (pre-eclampsia, fetal growth restriction, premature rupture of membranes, chorioamnionitis, failed antenatal testing). The reasons for early term delivery may be the cause of increased morbidity rather than the actual timing of delivery. Furthermore, environmental studies cannot legitimately comment on whether a specific identified pregnancy with multiple risk factors will achieve a better set of birth outcomes if delivered in the 37th, 38th, 39th, 40th or 41st week of gestation, and they cannot comment on the impact of moving a given patient from one cohort to another.
The second type of sub-optimal research is randomized clinical trials (RCTs) of elective repeat cesarean delivery. RCTs of elective repeat cesarean delivery have been done, and have shown that pre-39 week surgical delivery causes higher rates of adverse neonatal outcomes. These studies appear more compelling on the surface, but they should not be generalized to the setting of pre-39 week “non-indicated” labor induction. Elective cesarean delivery fails to expose the fetus to either the hormonal surges that occur during labor or the compressive forces that occur with both uterine contractions and passage through the birth canal. Both exposures prepare the fetus for extra-uterine life. Unfortunately, no adequately powered randomized clinical trials have been performed to measure the risks and/or benefits of risk-based labor induction in the 38th week of pregnancy. However, the AMOR-IAPT project has identified a cohort of over 300 pre-39 week preventive inductions, and the outcomes have been significantly better than neonatal outcomes in the general population. This information is included at the end of this document in poster format.
As a final thought, the two elements of AMOR-IPAT are probably interactive in a beneficial way. Early or mid-term delivery for CPD-related issues enables labor to occur when the fetus is smaller than it would be 1-2 weeks later, so labor is theoretically shorter and easier—and this might enable a normal delivery even in the presence of some utero-placental insufficiency. In addition, early or mid-term delivery for UPI-related issues enables labor to occur when the placenta is healthier than it would be 1-2 weeks later, so the fetus is theoretically able to tolerate a longer or more stressful labor—and this might enable a normal delivery even in the presence of fetus that is relatively large for gestational age but not too large at that gestational age to pass through the maternal pelvis. This interaction of benefits may be partly responsible for the fairly dramatic improvement in birth outcomes seen in cohorts exposed to AMOR-IPAT (see attached poster).
-----